Resources
Nephrology News & Issues • September 1999
Gathering Data in the Dialysis Unit: What Do You Need?
What Do You Need it For?
John A. Sargent, Ph.D.
Introduction
In the general rush to keep pace with advances in technology, the dialysis field has not been left behind. Payers are requiring more and more information from providers on substantiating the quality of their care. Implementing the National Kidney Foundation- Dialysis Outcome Quality Initiative recommendations, reporting to the End-Stage Renal Disease (ESRD) Networks, etc. has made dialysis facility managers who have not yet purchased computers uneasy. They are driven by the instinctive urge that “we must computerize.”
This article attempts to respond to those needs and add some perspective to this uneasiness by looking at how the dialysis industry has used technology over its 25+ year history. I propose that possessing data without the realization of increased knowledge severely limits their use and reduces the computer to the role of an electronic filing cabinet.
Dialysis is probably more quantitative than any other field in medicine, but to date, those in the field have not realized the potential of the information gathered. That is, we have not used our existing data to increase our understanding of what we do. There is enormous potential for using our data effectively to increase our understanding of clinical and business practices. It requires that we have the available resources to convert the masses of data and information in our possession into knowledge. Because of this potential, individual independent providers (i.e., those that can operate with considerable independence) have significant advantages over non-independent groups when competing on treatment quality and business issues.
The Advance of Technology in Dialysis
Looking back to 1973, when legislation was passed to create Medicare entitlement for ESRD, one can appreciate the advances that have been made in dialysis treatment. Table I shows several aspects of dialysis treatment in 1973 and compares it with their current status. A patient, the few for whom dialysis was available in 1973, received a six- to eight-hour dialysis using a coil or flat plate dialyzer that delivered urea clearances well below 200 ml/min. Individualizing of dialysate concentrations to address specific electrolyte or acid base problems was rare because central delivery was used. The patient could also go through significant acid base swings caused by the loss of serum bicarbonate and delayed metabolism of the acetate buffer. The treatment staff had a higher level of credentialing but the complexity of their job was greater due to the use of technologically unsophisticated equipment.
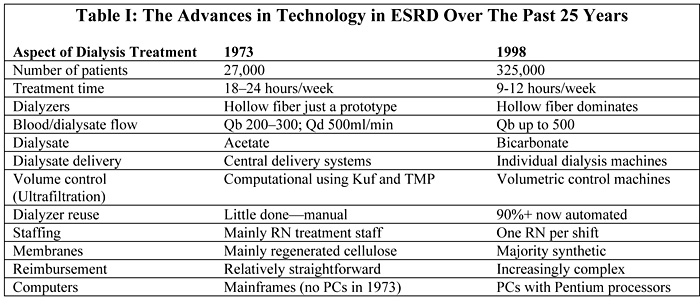
Although the advances since 1973 in dialysis delivery have been impressive, perhaps the most profound change in technology—not just in dialysis—has been the vast increase in computational capabilities (hardware and software) and their availability to everyone at affordable prices. Twenty-five years ago the personal computer (PC) didn’t exist. If one wanted to use a computer, they had to find access to a large university computer and computational time was purchased. Even though the changes shown in Table I are impressive, the greatest advances are in available computational technology. So how effectively has the dialysis industry used this technological opportunity? Not very well!
Much of the dialysis industry remains “uncomputerized.” Those who have purchased computers are often unimpressed or disappointed. In many facilities, given the choice of getting rid of the volumetric control machines or the computer system, the computer system might well be scrapped. Is this then just another indication that we are incapable of appreciating and using technology to operate more effectively? Not really. We, as an industry, have used advances in technology to improve treatment and reduce costs as illustrated by most of the items in Table I. In fact, the ability of this industry to continue to deliver dialysis at the same reimbursement levels with continually rising costs is in large part a result of the adoption of technical advances. The question is: Why haven’t computers been part of this solution?
Rule #1: Computers Convert Data Into Information—They Don’t Create Knowledge
A number of years ago Harvard Business Review conducted an interview with Walter Wriston, then CEO of Citibank. One of the quotes that appeared in that interview dealt with a fundamental problem with computerization that contributes to its slow adoption in the dialysis field:
“The incessant production of new data and its instantaneous communication creates a paradox. Information, the thing that eliminates uncertainty, now increases everyone’s feeling of insecurity because of the failure to convert information into knowledge.”1
Increased computational capability has not been embraced by the dialysis field. While it has provided more information, or the ability to get more information from roughly the same amount of data, it has not increased our knowledge and understanding of what we are doing. There are many facilities that have invested in computerization and have very little to show for it except frustration and extra work. Some insights follow.
Purchasing solutions before the problems are defined: Underutilization of computers has occurred in large part because those who purchased these computer systems had a vague idea that it would solve their problems without defining what those problems were. There has been the desire for some time to “become paperless.” What does that mean? Does it mean that there are no longer filing cabinets in the facility? It is unclear what computerized information would be used for beyond using the computer as a storage device. In the case of underutilized systems, it appears that they fell into disuse because they were bought as a solution before the problems were defined.
Support for this assessment of computers in dialysis comes from a study of information systems done as part of the Dialysis Outcomes and Practice Patterns Study (DOPPS). This study, initiated in 1996, seeks to evaluate practice patterns and outcomes using data from 161 dialysis facilities in the U.S. and overseas. Of these centers, 90 had computer software systems which covered the range from commercially marketed systems for medical records, lab reporting, and business needs to incomplete systems that addressed only labs or business applications. In an attempt to determine if these systems could be used for data collection for the DOPPS data, the facilities were surveyed regarding the systems that they used and their effectiveness.2 Partial results are shown in Table II.
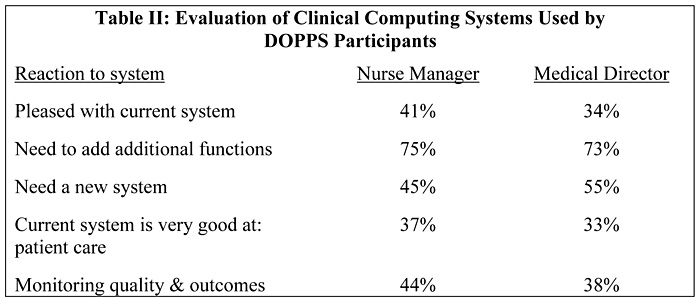
The systems in use were not necessarily bad. The lesson from Table II is that many of these facilities apparently bought their systems before they knew what they actually needed to do for improved job performance. When they actually started using them they found out that the capabilities didn’t fit the problems they were trying to solve. They had systems where the tools were unsuitable. And in reacting to the mandate that “we have to computerize,” they bought systems that didn’t meet their needs when put into practice. This is not a suggestion that we as an industry abandon the idea of using our data better to efficiently provide more effective treatment. It is a suggestion that the approach to using computers be rational and deliberate.
Building or Selecting a Computer System
The different approaches to using information should sort out the relationship between data, information, and knowledge. Such a relationship is illustrated in Figure 1a. Data is at the bottom and knowledge at the top of the pyramid. In this context, data are individual elements, such as blood pressures, dialysis times, dialyzer clearance, diagnoses, etc. Information comes from these data through computing relationships, sorting, compiling, presentation, etc. This step of taking individual elements of data and converting them into information is what computers are designed to do. Computers, however, do not give us knowledge, as Citibank’s Walter Wriston implies.
Knowledge, or increased understanding, comes from an individual looking at the information and recognizing an apparent pattern, raising questions, becoming curious about possible relationships, asking why the information seems counter-intuitive, and trying to explain it. They may also question the data or the manipulation that produced the information from the data. But it is important to recognize that without the top, the pyramid is of little use.
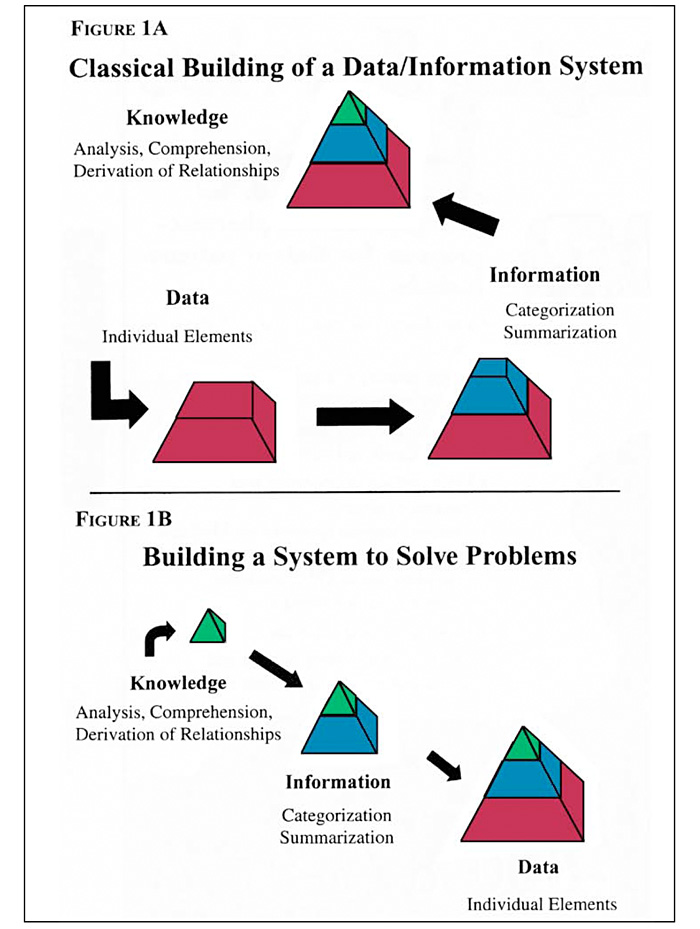
Figure 1 (A and B): Illustration of two different approaches to building a data system to solve problems and gain understanding and knowledge. A shows the methodical organization of data collection and computerization before addressing what knowledge is desired. B starts with consideration of the knowledge desired and works back to information to support it and the data required to produce that information.
It is common to build this metaphoric pyramid from the bottom up by collecting “everything” and putting it into a computer which will then spew out information. In medicine, this tends to be the impulse to collect everything—because once you have a database containing “everything” you may feel certain that this database can be used to answer virtually any question. When one has an insight or needs to answer a question, the data to answer it will presumably be there.
This approach is somewhat analogous to the camera in the bank that records everything so that when the bank is robbed you have a picture of the thief. In fact, this approach is wasteful and can’t assure that the data actually needed will be captured in a form that can be used to answer future questions. In dialysis, groups that tried to retrospectively analyze their databases after the conclusion of the National Cooperative Dialysis Study (NCDS)3 could not perform the analyses because pre-post urea levels had not been measured and were not in their databases.4
A better approach to the use of data and information when starting out is to build the pyramid from the top down (see Figure lb). This approach starts with deciding what knowledge is desired. Once this is known, the information that is needed can be determined and the data required to produce the information defined and collected. It is clear that this approach requires much less data and effort, and has much greater flexibility. The process is not controlled by the data and computational assumptions that would be inherent in the process described in Figure 1a. As the knowledge created indicates, different information is needed to better understand the problem; the data requirements can be altered accordingly.
Computer systems for dialysis have generally followed the classical approach, illustrated in Figure la, of collecting large amounts of data. This is indicative of the experience of the DOPPS participants, illustrated in Table II. It also explains why there has not been great enthusiasm by dialysis treatment staff in computerization. One would suspect that if computational capabilities are not used to increase understanding in this field, even though systems are purchased, the field will continue to miss the opportunities that greater understanding of clinical and business issues provide.
Rule #2: Define What You Want the Computer to Do
The potential for using computer technology in dialysis has been missed because we have not developed a clear definition of what we want it to do. In many ways, the field has, through unclear definitions of its specific needs, wasted resources by using computational tools that are not suited to specific problems. This waste of staff time and energy means that the potential gains from “working smarter” have not been realized.
Ignoring Knowledge That is Contained in Existing Data
As a result of the NCDS, the lower limit of dialytic adequacy was quantified in 1985 as a Kt/V of less than 0.8, with recommended treatment for all patients of 1.0 >Kt/V>1.2.3 A period ensued when many investigators searched their databases for retrospective data on dialysis adequacy, and there were several reports from groups who felt this value should be higher. But their findings were based on prescribed, not delivered, magnitude of treatment.4 As has been briefly discussed, they could not compute delivered treatment because they had not measured and recorded pre-post urea levels needed to compute delivered Kt/V (i.e., they had extensive databases, but those databases didn’t contain the data they needed). The concern for treatment adequacy was one of the factors that led to the Mortality/Morbidity Conference in Dallas in 1989.5 A report at this conference showed that there was a marked underdelivery of dialysis based on a comparison of prescribed and delivered Kt/V.6
As a result of this conference, several investigators decided to unilaterally increase dialysis treatment for all patients through various combinations of increased dialyzer size, increased blood flow, and by dialyzing for a greater period of time.7,8 The results of this study was a decrease in mortality when average Kt/V for the patient populations was increased from approximately 1.1 to 1.4. Figure 2 illustrates the results of these studies.
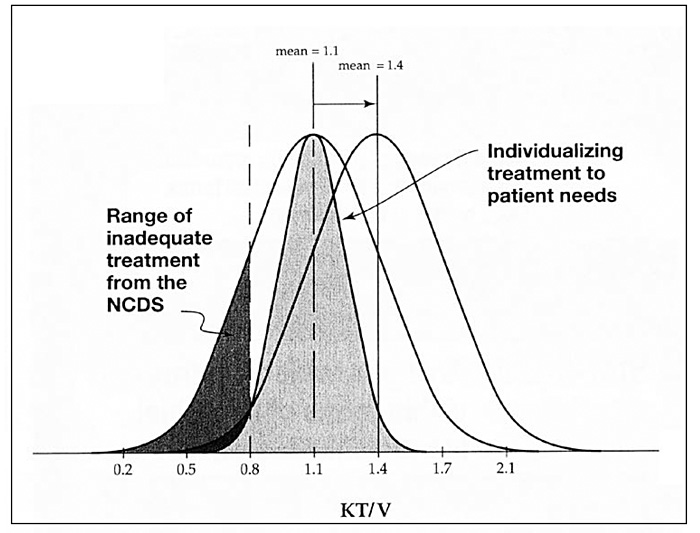
Figure 2. Analysis of data used to urge increased dialysis in the overall ESRD population in References 7 and 8. The means and spread of data are representative of the patient data reported in these references. The shaded distribution is used to illustrate a possible distribution if dialysis treatments are tailored to individual patient needs.
The wide, normal distributions shown accurately represent the distribution of Kt/V values for the study populations and, importantly, the range of this value from the highest to lowest values. The distribution on the left was the starting point with an average Kt/V of 1.1. When treatments were increased this average increased to 1.4 with the same spread of values. Clearly, in the baseline population, a large number of patients were receiving less treatment than had been determined as adequate during the NCDS (i.e., Kt/V > 0.8). When treatment was increased, the left tail of the distribution was moved to the right and a sizable number of patients were moved into the 0.8
However, from the figure it is clear that if Kt/V had been measured for individual patients, only those at risk needed to have treatment increased; the same improvement in treatment-related mortality could have been achieved keeping the average Kt/V at 1.1. The result of not using the knowledge available in the data was longer treatments, reduced quality of life for many patients who had to stay on dialysis longer, and greater expense because of the resources needed to provide more—and in many ways excessive—dialysis.
Had these investigators taken an approach guided by such knowledge, they would have avoided these negative consequences and would not have put data into the literature that less knowledgeable individuals, such as regulators and managed care directors, could use to dictate what treatment U.S. dialysis facilities must provide.
Using Automated Systems Not Designed for the Dialysis Problem
Dialysis is somewhat of an anomaly as a medical treatment. It is a chronic disease that requires active treatment. It is a catastrophic illness with large outlays funded from federal and state programs. As such it does not conform to normal medical care which is predominately for acute illness. Dialysis is also highly regulated (at least from a reimbursement point of view).
Normal delivery of medical care generally consists of an admission, some extent of treatment, and discharge. Most automated medical systems are designed for this sequence of events. Some of these, generally of a business nature, have been selected for use in dialysis. Because they are designed for other aspects of medicine these systems are often ill suited to the needs of the dialysis community. The result of using such systems can be costly omissions or tedious “work-arounds.” These difficulties waste resources and take time that could more productively be spent analyzing operations and increasing efficiencies.
An example of ill-suited systems exists in the hospital setting, where sophisticated business software, designed for acute patient care, is used for an outpatient dialysis program. In this setting, one often sees the need to repeatedly admit and discharge the same patients throughout a month, once monthly, or annually because the system demands this procedure.
There are other examples of systems that have been derived from general business programs or physician office software that impose constraints on the user based on the original design requirements for the base program. These solutions are generally selected because the problem—what data needs to be collected and for what purpose—has not been adequately addressed. This lack of initial definition reduces the level of analyses possible in the dialysis facilities, and places additional burden on the users due to the extra effort needed to accomplish the task with ill-suited systems. It is true that skilled individuals can use poor tools and get good results. It is unfortunate that such individuals are often frustrated, and not allowed to realize their full potential in helping the facility better compete in an increasingly tight field.
Where is Information Needed in Dialysis?
There are well-defined areas in dialysis where information is needed. The most recognizable ones are where outside groups or agencies require information. The requirements for information include:
- Meeting regulatory requirements: census information to the ESRD Network and 2728 form for the initiation of dialysis; and
- Justifying what we are doing (generally for payment): hematocrits for patients receiving EPO and Kt/V for hemodialysis patients.
It is unfortunate that the reports uniformly generated by the renal field and made available to others have been defined by outsiders and have not been initiated by the field itself (e.g., HCFA mandated that facilities measure and report “adequacy” parameters). It can be safely assumed that this may continue if we do not do. a better job of defining the problems that we must solve and what information we need to effectively address the problems.
For the long-term survival of ESRD providers, information should be used to produce knowledge which can form the basis of clinical decisions, and as a foundation for operational and business decisions. As has been discussed above, this information will depend on the knowledge needed by individual providers and not necessarily what is mandated uniformly by outside agencies. This information has the potential of being far more useful because it will be determined by the actual user of the knowledge to help them address pressing local problems. The ability to define these problems and craft strategies to solve them depends on the availability of motivated personnel with time and energy to devote to these tasks. The lack of effective tools for jobs that are already defined wastes staff time and frustrates this effort.
Knowledge for the Independent Dialysis Provider
The independent provider in the context of this discussion does not refer to the ownership of the dialysis facilities, but to the management and business model under which they operate. This class of dialysis provider, if they use information effectively to gain increased understanding of the wide range of problems that confront them, can be a more effective competitor than groups that are not so organized.
The local provider knows the local environment and demographics of their community and can react to changes quickly. If they are truly independent they will have local “ownership” of the processes and analyses. They will also have the liberty to define the problems they feel are in greatest need of solutions (e.g., they may feel they have a greater problem with volume control than access and want to solve that first). The independent provider also has control of their data and analyses and can have a tight information loop.
As previously discussed, it is important to define what knowledge one wants to gain before starting computerization. Once sought after knowledge is defined and information to support it is determined, it is critical to collect and analyze the data quickly. The maximum benefit of feedback is achieved when the accuracy of the collected data is determined immediately and needed modifications to the data collection process are rapidly incorporated.
Some attributes of a tight information loop are:
- Collect only the information that you need (see Figure 1b). Collecting too much data wastes resources and saps the enthusiasm of staff. It may make the project inflexible and can compromise the accuracy of the data that you actually need.
- Perform analyses immediately. Rapid analysis allows one to check assumptions and determine if the data are producing the information and elements of knowledge that is the goal of the project.
- Supply the results to those who need them rapidly and on whose efforts you rely on for its accuracy. For example, in a research context, the most critical step is assuring the quality of the raw data. Operational information should be based on no lower than a data quality standard. If those collecting it have no stake in its accuracy or don’t understand what they are collecting it for, their commitment to its quality will be diminished. Often if there are problems with understanding the results, the person who actually obtained the data can supply crucial details to improve the process.
- Retain flexibility in the collection and use of the data. Often it is not possible to know what data will be required and how it must be analyzed. Collecting too much and following inflexible protocols frustrates the use of information. It is important to go where the analyses lead and not be restricted by an approach that limits flexibility (see Figure la).
Independent dialysis providers often operate in isolation. It is important to be able to compare your results to national numbers in order to assess how your operating parameters compare to the industry at large. Benchmarks are not generally available from a single source. The U.S. Renal Data System (USRDS) provides some benchmarks on mortality; others are available from ESRD Networks and independent providers. It is important to seek comparisons for fundamental operating parameters—both clinical and business. Some benchmarks that may be of interest are missed treatments due to hospitalization, revenue per treatment, revenue from the major components of the treatment, hematocrit, Kt/V, etc.
Summary
It is clear that the use of information has not been adopted by the dialysis field as rapidly as other technological advances. Even when computer systems are used the collection of data has often be viewed as tedious. Those collecting it often don’t see that it is effectively used and it commonly does not help them do their jobs. In short, the data and information that the computer generates is not used to create knowledge or increased understanding of problems to be solved; in many cases it does nothing to make tasks easier or help staff provide good care on a daily basis.
The lack of knowledge has been the result of the lack of definition of the problems that need to be solved. In areas where the problems are defined, which are mainly business problems, computers are normally used effectively, as long as the systems employed are specific to the task. Nonetheless, because we have not defined the problems, we have not exploited the vast increase in computing capabilities that are available. In most cases we have missed opportunities to more effectively manage ESRD care, clinically as well as operationally. But worse yet, in those cases where data, information, and knowledge have not been exploited, it has resulted in increased costs because of not “working smarter” (e.g., unilaterally increasing treatment; see Figure 2).
The potential for information, while fundamentally unrealized to date, will always exist. The value of information is probably greatest on the local level where specific clinical and business problems can be defined and analyzed rapidly using current computational technology. Effective use of information on this scale represents the single most effective tool for the continued improvement of ESRD care and the survival of independent dialysis providers.
References
- 1. Wriston W.B.: “The world according to Walter.” Harvard Business Review 64(1):65, January-February 1986.
- 2. Young E: DOPPS data survey; personal communication.
- 3. Gotch FA and Sargent JA: “A mechanistic analysis of the national cooperative dialysis study (NCDS).” Kidney Int 28:526, 1985.
- 4. Collins A, Ma J, Umen A, Keshaviah P: “Urea index and other predictors of hemodialysis patient survival ”Am J Kidney Dis 23:272-282, 1994.
- 5. Parker T, ed: “Dallas morbidity and mortality conference.” Am. J Kidney Dis Vol. 15, 1990.
- 6. Sargent JA: “Shortfalls in the delivery of dialysis.” Am J Kidney Dis 15:500, 1990.
- 7. Parker T, Husni L, Huang W, Lew N, Lowrie E, Dallas Nephrology Associates: “Survival of hemodialysis patients in the United States is improved with a greater quantity of dialysis.” Am. J Kidney Dis 23:670-680, 1994.
- 8. Hakim R, Breyer J, Ismail N, Schulman G: “Effects of dose of dialysis on morbidity and mortality.” Am J Kidney Dis 23:661-669, 1994.