Resources
Dialysis & Transplantation, April 1991
Cost-Effectiveness of Computer Solutions in Dialysis
John A. Sargent, Ph.D.; Richard A. Clark; Michael Paget; William W. Kingston
John A. Sargent, Ph.D.; Richard A. Clark; Michael Paget; William W. Kingston
Computer technology can now be applied to virtually every aspect of dialysis-care delivery; however, analysis and judgment are required to determine which applications will be cost-effective for a specific facility and how they can best be implemented. Costeffectiveness must be considered, since arbitrary limitations on the cost of care are an increasing reality.
Cost-effectiveness can be quantified as the amount that the value of the application exceeds the cost of implementing it. Value can be computed by considering savings in labor costs, increased staff effectiveness, and benefits of improved quality-ofcare delivery. If computer applications are purchased as a service, cost determination and cost-effectiveness analysis are straightforward. If, however, computer applications are done on an in-house basis, the analysis must consider the total costs, including those which might be considered “hidden.”
Determination of the right degree of automation for a particular facility considers both the value and affordability of the proposed approach. An analysis has been performed for a hypothetical facility at three candidate levels of automation. Estimated total costs for in-house implementation are compared with estimated costs for equivalent purchased services. (Such comparisons are increasingly possible because task-specific computer applications can now be linked using telecommunications to provide an integrated system solution.) In this comparison, the typical savings realized by purchased services exceeds 50% of the comparable in-house cost.
The approach used here can be applied to any specific facility by defining the capabilities to be implemented, then evaluating the total cost of in-house implementation as compared to the cost of equivalent purchased services.
GETTING STARTED
The dialysis field is moving toward greater and greater automation.[1-9] This move can be seen in microprocessor-controlled dialysis-delivery machines,[10] as well as several data-base—type systems designed to computerize medical records.[3,7,8] These latter systems offer the promise of organizing patient data for easy retrieval to assist in the management of patient care.[3,7-9] In addition, some systems are advertised as “paperless,” to promote elimination of the patient record as it is now known and used.
These computer applications are only a part of what is available in automation and increasingly desired by computer users in dialysis facilities (see Table I).
Table I: Some automated features increasingly desired by dialysis facilities
Microprocessor control of dialysis machines
Computerized medical records
Computerized laboratory results
Word processing
Computerized payroll
Computerized inventory and purchasing
Computerized general ledger
Computerized billing, accounts receivable, and submission of claims to secondary payors
Electronic submission of claims to Medicare intermediary
Electronic submission of claims to Medicaid
Computerized cost-reporting to Medicare
Computerized urea kinetics and quality assurance
Computerized guidance and surveillance of EPO
Computerized data-base and spread-sheet analysis
Computerized drug-drug and nutrition-drug interaction
Computerized nutritional (diet intake) analysis
Electronic mail
Once the decision is made to automate, the way in which it’s achieved is important. There are at least two aspects to consider: How much of the facility should be automated? What is the best way to go about it? Also of importance is whether you should buy an in-house system, including hardware and software, and operate it with facility staff, or buy targeted solutions on existing supported off-site computers.
This paper investigates the means of determining the cost-effectiveness of automation, and explores the economic value of alternatives to automating dialysis facilities.
Cost-Effectiveness of Automation. Reimbursement in the dialysis field has continued to decrease in real terms, while costs continue to rise. Automation has great potential to reduce costs and improve quality of care, but not all applications may be costeffective. It is, therefore, critical to evaluate the increase in value that will result from implementing a particular capability in relation to its costs. Specifically, it is important to determine:
- How much will automation cost?
- How much will automation save, or what increase in value will result?
- Is automation worth the cost?
- Is automation affordable?
Determining Cost-Effectiveness. It’s possible to evaluate the cost-effectiveness of automation by using the relationship shown in Equation 1:

If cash flow from competing alternatives is relatively similar, dividing Equation 1 by “Cost of Automation” yields a simplified expression for return on investment (ROI), as shown in Equation 2:

Note that in using Equation 2, the ROI “cost” is the total cost of automation, not just the capital portion of that cost.
It’s apparent from Equation 1 that, for automation to be an effective addition to dialysis (i.e., the left side of Equation 1 positive), “value;’ or benefit, should exceed “cost.” Our approach is to define and evaluate the elements of the two terms on the right of Equation 1. It is also important to evaluate ROI (Equation 2), and the results of these two calculations should guide the decision to automate.
In a field like dialysis, where margins are shrinking, it’s particularly important to consider the amount by which the benefits exceed costs (i.e., the difference of the two terms on the right of Equation 1). If the ROI in Equation 2 is reasonable, the amount of benefits is more important than the actual cost of automation. In other words, automation that costs $50,000 and results in $60,000 in benefits is superior to one costing $5,000 and producing $6,000 in benefits, even though they have the same ROI.
Value of Automation. The value of automation is the combination of both quantifiable and less tangible factors. That is, many computerization applications can reduce costs, while others produce increased quality or ease in accomplishing specific tasks.
Computers are widely viewed as being able to decrease labor costs and improve staff efficiency (i.e., a priori, computers are cost-effective). Automation in specific settings has been shown to produce this effect. Word processing increases the quantity of work one person can perform and reduces staff time required to manually retype documents; computer production of Medicare bills saves time and reduces administrative staff workload. Greater staff efficiency is also realized in increased nursing effectiveness resulting from using microprocessor-driven dialysis-delivery machines that centrally display and record treatment information.[10]
Computers also have value in that they improve the quality of work produced. Historically, word processing was employed to reduce labor costs. The real value of word processing, however, has more often been realized in improved quality of output because of the ease of making document revisions. This has been deemed “worth the cost,” even without realizing any cost reduction.
Another value of computers, which is difficult to quantify, is their ability to enhance clinical or administrative capabilities. Such enhancements include increased control over operations using data-base analysis of information. For example, clinical data bases are able to generate reports of historic laboratory results for patients or develop other analyses that can increase the quality of care, although not necessarily decrease the cost of delivering it. Similarly, using urea kinetics to determine whether therapy is fully delivered[11] and adequate[12,13] may require some additional staff time, but vastly increases the utility of clinical data.
A summary of the value of automation in dialysis is shown in Table II, and the process of balancing those elements of value against the costs is illustrated in Figure 1.
Table II: Various elements of value for automation in dialysis
Saves labor
Allows staff to do more
Avoids mistakes
Gives ready access to data (financial/clinical)
Allows clinician to monitor treatment (delivery/adequacy)
Permits better viewing of clinical data
Makes medical record available in different locations
Improves patient throughput
Helps to market unit to physicians, staff and patients
Gives staff prestige in field
Provides data for technical papers

Figure 1: Cost-effectiveness is the balance of value and cost of automation
COST OF AUTOMATION
The cost of automating includes hardware and software purchase, as well as the associated costs of support and maintenance of computer systems. These costs may include: buying equipment, buying or leasing software, and retaining staff and services to run the hardware and software. As we see in Table I, there are many types of automation. There are also different means of automating some of these functions, such as using outside data processing or in-house mini-computers, or adapting existing office equipment.
Specifically, outside data processing will generally address some well-defined aspects of automation (e.g., billing, payroll). In-house systems tend to offer computing solutions to multiple automation applications using the same system, although purchasers can often select which applications they want. With this array of features, the total system costs (purchase price, support, internal staff requirements, etc.) will vary, depending on what the system is intended to do. To make valid intersystem evaluations, similar features should be compared, with extra features being evaluated separately. If this cannot be done, Equation 1 should be applied to each system to determine overall costeffectiveness. That is, if an outside billing service costs $20,000 and provides benefits worth $60,000, it is a better choice than a more complex system costing $50,000 and producing $65,000 of benefits. (In other words, the other features cost $30,000 for $5,000 of additional benefit.)
Analyzing Costs of Outside Data Processing. Automated data processing supplied by outside systems generally targets specific areas where these services offer significant benefits over in-house computers, and where special expertise and support are needed. 14 These include payroll and billing. Outside data processing is provided on a fee basis, making total costs for a specific capability easy to determine from supplier quotations.
Outside data-processing costs are generally based on a fixed account charge, with additional usage costs determined by the time the service is used, by the amount of data stored, or by some other measure of system utilization. Support and maintenance of the software are generally included in the account charge, as are telecommunication costs. For these systems, as usage increases, overall cost increases; however, per-item costs, cost-per-patient or cost-per-treatment, decreases.
Analyzing Costs of In-House Computer Systems. In contrast to outside data processing, the costs of in-house computer systems are more difficult to evaluate because they fall under different items in a facility’s budget. These items include equipment and software purchase, equipment and software maintenance, vendor support, and system management and programming personnel. Some in-house systems, such as patient medical-record systems, may also require increased staff for data input.
Hardware Costs. Evaluation of the total cost of in-house hardware must consider purchase, maintenance, and the useful life of the equipment. Annual costs for hardware are determined by allocating the acquisition or lease expense over the useful life and adding the annual maintenance fees. If the equipment is purchased, the acquisition expense must include the time value of money. If the equipment is leased, the time value is built into the lease expense.
In determining the useful life, it must be recognized that computer equipment rapidly becomes obsolete, due to the pace of development in this field. New equipment will be needed or desired within a few years of the initial purchase. For example, updated operating systems may be needed for subsequent releases of software and may require enhanced hardware capacity; older equipment may go off maintenance and require upgrading of specific components. In addition, system use may outstrip the capabilities of the original hardware. Experts in the data-processing field estimate that PC and minicomputer hardware has a maximum life of 36 months. Our experience with medical computer applications indicates that a three-year turnover (renewal) for computer hardware is realistic.
Hardware maintenance is generally a monthly or annual fee, and usually approximates 1% of the purchase price per month (10%—15% per year).
Software Costs. The analysis of software costs is similar to that for hardware. The useful life analysis recognizes that some applications software becomes obsolete very quickly. In billing, for example, dialysis reimbursement regulations and their interpretation by intermediaries change frequently (e.g., payment for erythropoietin-EPO, or Gramm Rudman adjustments). In those cases, even though the software may be errorfree, it becomes less usable. Accounting and administrative software may have a somewhat longer life, although the rate of change in those areas is also significant. An estimated average life for dialysis software is 24—36 months.
Software maintenance covers error correction in purchased software. These errors are “bugs” that were not discovered during development due to inadequate testing, or result from use of the software in a manner that was not considered during its design. This type of maintenance requires the availability of programming staff who are familiar with the design of the purchased code. The maintenance of dialysis software is further complicated by the fact that each copy of the software may be slightly different, with its own set of “bugs,” as a result of different intermediary requirements. The maintenance cost for dialysis software is expected to be l0%—15% of the purchase price per year.
OPERATING COSTS
User Support. Support is providing “user-friendly” people to help facilitate software use. This task includes helping users locate appropriate operations so the software gives them the information they want, such as customized reports that address specific needs of a wide spectrum of facility staff. In addition, support is required to modify programs, to address changing reporting requirements in dialysis and to assure their continued usefulness pending the next version of the software.
Vendors may supply some support. The quality of this support will depend on how familiar vendor personnel are with the software (i.e., a knowledgeable and experienced programming staff), being familiar with the specific application (e.g. dialysis billing), and having the customer software as a primary professional responsibility.
Our experience with systems that require intensive support, such as billing, is that each user organization will require 0.10 to 0.15 full-time employees (FTE) to provide software support. At commercial rates— $80—$l50/hr — this level of vendor support would cost $20,000 to $25,000 per year. Consequently, the customer may use the vendor for high-priority items only (0.5 to 1.0 days per month), at a cost of $5,000 to $10,000/year.
These figures do not include all support, partly because the user avoids other than major support needs due to hourly costs. In addition, there are certain support tasks that are best done by those with ready access to the software. Therefore, vendor support, if provided, will have to be supplemented by an on-site system manager.
System Manager. To operate an in-house system, look for a local individual who is skilled and knowledgeable with the system, and who can conduct local maintenance and support functions. These functions include checking status of terminals, backing up files, and acting as a resource for other users regarding features of the system.
For more complex systems, (e.g., paperless clinical systems), the system manager would also be responsible for controlling system use (e.g., setting up system security and assigning passwords), restarting terminals that are “stuck,” as well as arranging for maintenance of remote terminals and communications links. He/she is also responsible for setting up database listings: nurses’ comments, billable items, prescriptions, physician rosters, staff lists, etc. This person supervises entry staff to assure that information is current, determines hardware needs and deals with all necessary vendors.
This individual also provides secondary training of staff in turnover positions, as opposed to primary training initially provided by the vendor, and acts as software vendor contact for maintenance items and new features that are desired. He negotiates the price of revisions with vendors.
Although not quantified for this analysis, provision must be made for a backup for the system manager in the event of illness or vacation, as well as for problems resulting from staff turnover. This is especially critical in a small operation and may be the deciding factor in choosing not to bring equipment in-house.
The time commitment required for the system manager can vary significantly, due to the wide range of tasks. Our estimate is between 0.25 and 1 FTE, depending on the size and complexity of the application. If the vendor does not provide support, 0.1—0.3 FTE of vendor support must be incorporated into the system manager’s job, for a total of 0.35—1.2 FTE. Alternately, a part-time programmer could be substituted for vendor support.
Downtime. Most vendors acknowledge that their system will have certain “down” periods because of hardware malfunction or software problems. In addition, systems must be taken out of service to install or test software upgrades. There is clearly lost time when the system is not available to its users. Depending on the nature of the system (e.g., paperless clinical systems), several key employees may have to suspend their normal tasks and vendors summoned on an emergency (premium rate) basis. In addition, there may well be lost data, and, depending on the backup schedule, data may have to be re-entered.
Once system functions are restored, the task of catching up may take several days and require some premium time. Personnel requirements will vary between applications, but, if one outage involves five people for a total of two days each, two outages a year would require 0.08 FTEs. One can imagine even greater difficulties concerning vendors without access to user software or disagreement about the cause of system failure (hardware or software), resulting in delays in determining the cause of an outage. These delays simply add to the time required for resolution of the underlying problem.
ADDITIONAL COSTS
Although not quantified for this analysis, facility costs for space, power, surge protection, systems management, and space for the vendor to complete repairs and updates must be included with in-house costs. In addition, careful management is required to avoid other potential major costs. Examples include: costs of correcting for inadequate system design, inadequate maintenance and inadequate training. Ironically, these deficiencies will often increase staff costs for simple tasks that automation was intended to eliminate, such as increased manual production or adjustment of bills. Further, some dialysis-system vendors have left the field, either going out of business or shifting to other areas of software development. When that happens, the vendor-supplied services and support are no longer available. This can have a dramatic economic impact on the cost of an in-house system.
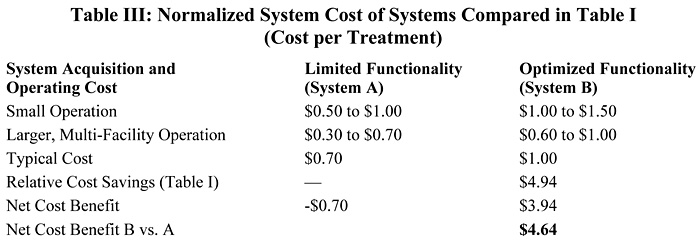
In-House System Costs. The examples presented in Table III illustrate a possible range of clinical/business systems for a dialysis facility and its annual costs. “System A” would be an extensive system with complex software. This is a possible example of integrated clinical and billing systems that are typical of a totally computerized dialysis center. “System B” is more modest. It might have some clinical capabilities, but it is not a “total” system. “System C,” in our estimation, is between the middle and low end of a billing system having no clinical applications.

COMPARING METHODS OF AUTOMATION
Billing Comparison. To make the data in Table III more meaningful, consider the automation of the reimbursement section of Table I for a facility with 100 patients. The specific computerized elements for this comparison would be billing and accounts receivable. Outside data-processing solutions exist for this particular application. There are also several in-house systems that address this application. Such systems can be reasonably well represented by “System C” in Table III.
The comparative costs of these two means of computerizing billing and dialysis reimbursement are presented in Table IV. It’s apparent that some types of costs, such as hardware, are common to each system. In this case, the difference is that the hardware required to use outside data processing generally consists of a modestly priced personal computer and modem, while in-house systems require more equipment to meet processing and data-storage requirements. As we’ve discussed, charges for most other computer-related costs of in-house systems are included in usage fees for outside data processing. Consequently, the in-house costs of system software, software maintenance, vendor support, systems management personnel and downtime must be compared to the cost of these items supplied as a service by the outside data processing organization.
Comparative hardware costs for these two means of automated billing are not unexpected. It’s clear that to do all data processing in-house requires more hardware than having someone else do it. In this comparison, the added annual hardware cost is approximately $8,000.
Perhaps more surprising is that “hidden costs” —costs that are not generally considered when estimating the cost of automation—increase the cost of using in-house systems more than $14,000 over the comparable costs of an outside data processing service. The total cost increase, when adding in the more expensive hardware, is more than $22,000 for this 100-patient facility. It should be pointed out that this comparison assumes the two capabilities are the same, that bills can be produced rapidly and accurately, and that management of collections and follow-up are comparable. Note that, if other unquantified costs for in-house systems were included, the comparison would be even more in favor of purchased service.
General Applications Comparisons. The foregoing has considered just one item from Table I. It’s clear that to more fully implement the automation in that table requires considerable in-house capability, with costs similar to “System A” in Table III. A look at Table I shows that even “System A” is not a total solution. For example, it would be impractical to consider the use of an in-house computer to control dialysis machines. Dialysis-machine manufacturers have addressed this problem and have basically solved it. Similarly, word processing is state-of-the-art and is available in many inexpensive software packages for personal computers.
For more comprehensive automated systems, therefore, analysis of costeffectiveness should consider the advantages of a hybrid approach. That is, prospective buyers should approach the decision for each element of Table I individually, considering value and costs and, consequently, cost-effectiveness of each item. As discussed earlier, not all items, as defined by Equations 1 and 2, will be cost-effective as stand-alone systems on a strictly cost basis. However, the greatest cost-effectiveness for a combined system can be achieved by selecting the best alternative for each application, which is the essence of the hybrid approach.
CONCLUSIONS
The dialysis field is becoming more comfortable with computers, and automation is, in a general sense, considered “state-of the-art” when planning a new facility. The widespread assumption is that to computerize is to be at the forefront of technology and is crucial to providing cost-effective dialysis therapy.
This analysis provides a framework to examine the latter assumption—that computerization is cost-effective. Specifically, it has reviewed the definition that cost-effectiveness results when increased value exceeds increased cost. Some of the value of computerization can be measured in labor savings; other aspects of “value” are more difficult and are manifest in increased quality or convenience. In addition, it is generally felt that a more “modern” facility will attract and retain physicians and patients. Consequently, the value side of the cost-effective balance contains elements that may be difficult to quantify; however, these should be honestly assessed by the facility.

Figure 2: The cost of in-house automation must include many other expenses in addition to the purchase of hardware and software.
The cost of computerization is easier to evaluate because many elements of automation costs can be calculated (e.g., purchase cost, maintenance cost, extra personnel, etc.). Others present greater difficulties (e.g., the cost of downtime, implications of inadequate design or training, or vendor business failure).
Automation also comes in various forms: shared supported systems for specific applications like payroll and billing, and complete purchased systems. The cost of the former is easily evaluated because services are billed for system use. The cost of the latter is considerably more difficult due to the number of “hidden” costs.
Hardware and software vendors commonly claim that the cost of such systems is simply the purchase price (see Figure 2). Our analysis shows that “hidden” costs are commonly almost 200% of the prorated purchase price (based on industry estimates of a three-year life for hardware and software). To answer some of the questions addressed at the beginning of this analysis:
- Is automation worth it? It depends on the balance between value and cost. For some applications, such as billing, payroll, general ledger, and other areas of administrative concern, it may clearly be worth it. There are other areas where the computations shown in Equations 1 and 2 are difficult, such as clinical data records and clinical computation (e.g., urea kinetics). These applications have the potential of improving quality of care, but their value is less quantifiable, as are other areas like making facilities more “marketable” to staff and patients.
- How much will automation cost? The answer to this question has formed the basis of this analysis. The total cost for in-house applications includes costs not normally allocated to computerization, as well as the cost of factors like the real life of computer hardware, software, and on-site management of the system that are commonly underestimated or dismissed (see Figure 2).
- Is automation affordable? With a realistic view of the added value to be achieved by automation of specific tasks, and a clear view of the cost of automation, the answer is readily apparent. It should be noted, how- ever, that the answer need not be “yes” or “no.” Although large systems may require an all-or-nothing decision, appreciating that different tasks require different solutions may permit facilities to have most of what they need at a reasonable price.
Acknowledgments: The authors wish to thank Edmund C. Lowrie, MD, of National Medical Care (NMC), Waltham, MA, for his help and suggestions regarding the content and presentation of material in this paper. We also thank Robert Burkhardt of Automated Data Processing (ADP), Roseland, NJ, for his input on in-house system costs, and Noel Tebo, Management Engineering consultant, San Jose, CA, for his review of and suggestions for the article.
REFERENCES
- 1. Knapp MS Stead WW, eds. Computing in clinical nephrology. Kidney Int 24(4):433—525, 1983.
- 2. Cheek D, Zasuwa C, Levin NW. A practical algorithm for blood pressure (BP) monitoring and control during hemodialysis. Trans Am Soc Artif Intern Organs 30:189, 1984.
- 3. Ash SR. A review of automated clinical records in nephrology: Can clinical records problems be solved? Contemporary Dialysis and Nephrology 7(1):40, 1986.
- 4. Williams MA. Computerization of the dialysis unit: Is buying software an easy decision? Contemporary Dialysis and Nephrology 7(1):33, 1986.
- 5. Johnson AW. Shopping for a computer for your office/facility. Contemporary Dialysis and Nephrology 7(1):34, 1986.
- 6. Shriver J. Computers help with diagnoses. Contemporary Dialysis and Nephrology 7(1):39, 1986.
- 7. Stead WW, Garrett LE, Hammon WE. Practicing nephrology with a computerized medical record. Kidney Int 24(4):446, 1986.
- 8. Pollak V. Computerization of the medical record: Use in care of patients with endstage renal disease. Kidney Int 24(4):464, 1983.
- 9. Stead WW. Evolution of technology brings computers to the bedside. Kidney Int 24(4):436, 1986.
- 10. Peterson G. Computer assisted quality assurance. ANNA Journal, April 1991.
- 11. Sargent JA. Shortfalls in the delivery of dialysis. Am J Kidney Dis l5(5):500, 1990.
- 12. Lowrie EG, Laird NM, Parker TF, et. al. Effect of the hemodialysis prescription on patient morbidity: Report from the national cooperative dialysis study. N Engl J Med 305:1176, 1981.
- 13. Gotch FA, Sargent JA. A mechanistic analysis of the national cooperative dialysis study (NCDS). Kidney Int 28:526, 1985.
- 14. Fersko-Weiss H. The return of outside data processing: Service companies turn to new applications in vertical markets for growth. High Technology Business, p. 41, December, 1987.
- 15. Sargent JA, Grutze A, Ontiveros C. Cash flow and accounts receivable management for dialysis. Dialysis & Transplantation 13(4):201, 1984.